New CIHR grant to implement findings of visioning document
As Paramedicine looks to the future, a UTSC Professor is at the forefront of efforts to guide the profession through a period of flux.
Assistant Professor Walter Tavares is the supervisor of the Department of Health and Society’s redesigned Specialist Program in Paramedicine, which is administered jointly with Centennial College. Prof. Tavares, a paramedic, researcher and leader, who himself graduated from the joint program, has dedicated his career to helping the Paramedicine profession contribute to overcoming healthcare challenges in Canada.
Paramedicine has changed in recent years, notes Dr. Tavares. “Paramedicine’s role in the healthcare system has broadened significantly, initially in the emergency/urgent care paradigm, but more recently in a variety of ways that can be collectively described as community-based health and social services. Increasingly, paramedicine is being called upon to do more to support our ongoing healthcare crisis, to rethink its guiding principles and paradigms, and links to health policy. For example, paramedicine is now being considered as part of interprofessional primary care teams, paying more attention to social determinants, to rethink how it is and can be accessed by the public, and to better align services with the needs of the community, patients they interact with and community resources that may or may not be available. This changes what we mean when we say paramedicine, including educational needs and supports.”
COVID was also a big catalyst for change. With Paramedics heavily involved in screening and vaccinating, Dr. Tavares says, processes of change already underway in the healthcare system were accelerated.
Dr. Tavares was a lead author on a visioning report commissioned by the Paramedic Chiefs of Canada, published in June 2023, which examined Paramedicine’s role in the larger healthcare system given increased demands and a growing focus on community based health and social services and a need to better integrate healthcare services across the country.
This shift towards community based health and social services, access and continuity of care, is at the forefront of the changing philosophy of Paramedicine, says Prof. Tavares. This is not only a focus of the visioning report, but the impetus behind the move of the Paramedicine program from Biological Sciences to the Department of Health and Society, aligning with the changing focus of the profession.
“There's a shift in the profession that's not quite complete,” notes Dr. Tavares, “and I think the move to Health and Society helps to recognize that that shift is underway and to participate in that, and to help guide it. Focusing Paramedicine under the philosophy of the Department of Health and Society aligns well with not just what the discipline needs, but with the direction of the healthcare system, which is more focused on decentralizing healthcare, for more integrated, and team-based healthcare delivered in the community.”
The visioning report titled “Principles and Enabling Factors Guiding Paramedicine in Canada: A Community-Based Healthcare System” identifies ten principles and six enabling factors intended to guide system design.
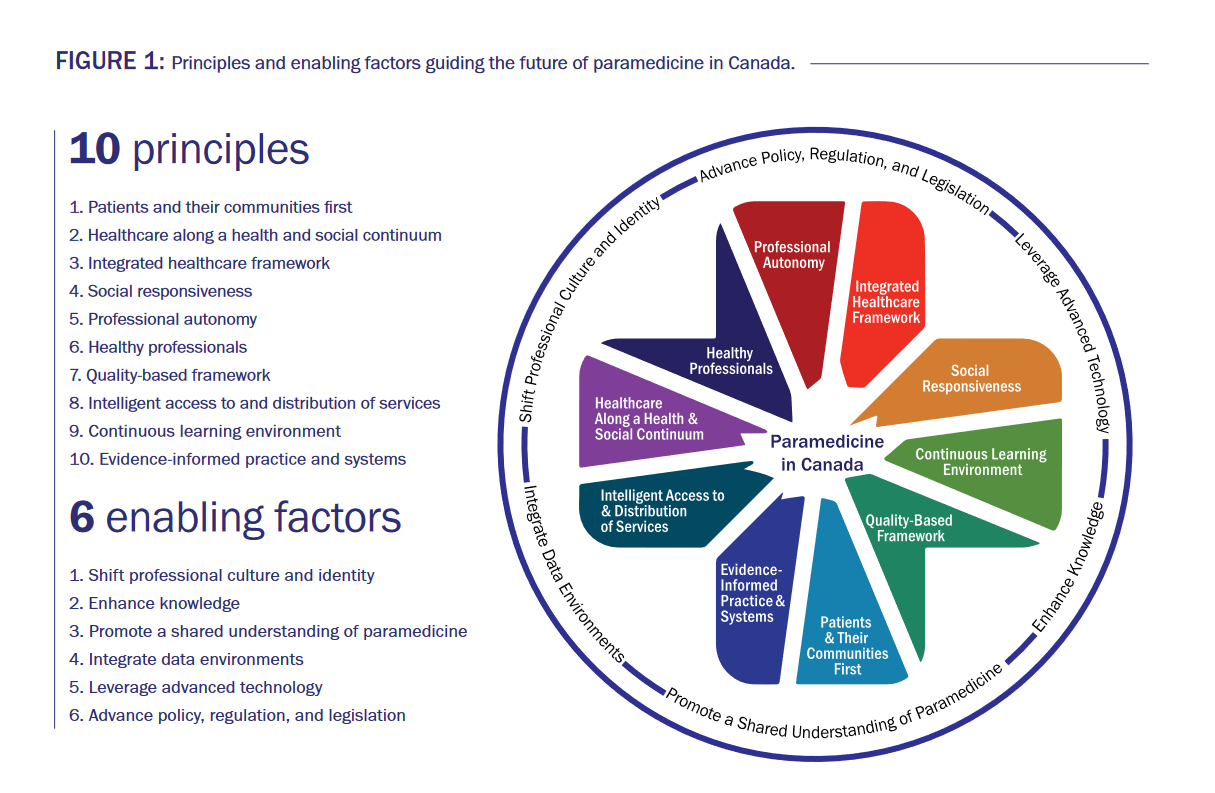
Many of these changes are already underway, notes Dr. Tavares. For instance, earlier key performance indicators that have focused on response times are now being reconsidered for other quality-based frameworks, that include for example, patient experience and clinical outcomes. The principle “social responsiveness” is placing a spotlight on issues such as gender bias in leadership roles in Paramedicine, including steps to be taken to improve inclusiveness.
The report is also shedding light on what Dr. Tavares has described as enabling factors in the report, one of which includes the sharing of data between systems and services. “Currently, we don't have a system where the neighboring paramedic services can share data with each other, or with other healthcare partners,” notes Dr. Tavares.“This is limiting the ability to conduct meaningful and much needed health system level research and quality initiatives”.
It is these kinds of systemic challenges, the enactment of the principles outlined and the need to focus on key enablers that Dr. Tavares hopes to resolve with a new grant from the Canadian Institutes of Health Research entitled “Redesigning Paramedicine in Canada”. This project aims to start the process of translating the visioning report into actionable steps and to set up future operating grants around these principles and enablers. ”This funding will bring together experts and researchers from across the country to guide the profession and its partners in how best to action the principles and enablers, and to begin or in some cases continue the process of change,” says Dr. Tavares.
Dr. Tavares acknowledges the efforts of many collaborators on the new framework, the Paramedic Chiefs of Canada and York Region Paramedic Services. He is also acknowledges the expertise of a variety of researchers and experts via the McNally Project for Paramedicine Research, which he co-chairs. Dr. Tavares initiated this research capacity development project in 2014 after completing his PhD in 2014. Since then it has grown into a Canada-wide community with 120 paramedic researchers.
“The McNally Project is now a collective of paramedicine researchers who share an interest in and vision for advancing paramedicine through research,” says Dr. Tavares. “We’re seeing that translate into exceptional research capacity in the system that we now hope to leverage as part of this new CIHR funding. We hope to engage students in these opportunities as a way of supporting their development and future contributions.”
